Improving Outcomes of fragility fractures in North East London’s ageing population through data-driven rehabilitation
As North East London’s population ages, the region faces a growing challenge: fragility fractures.
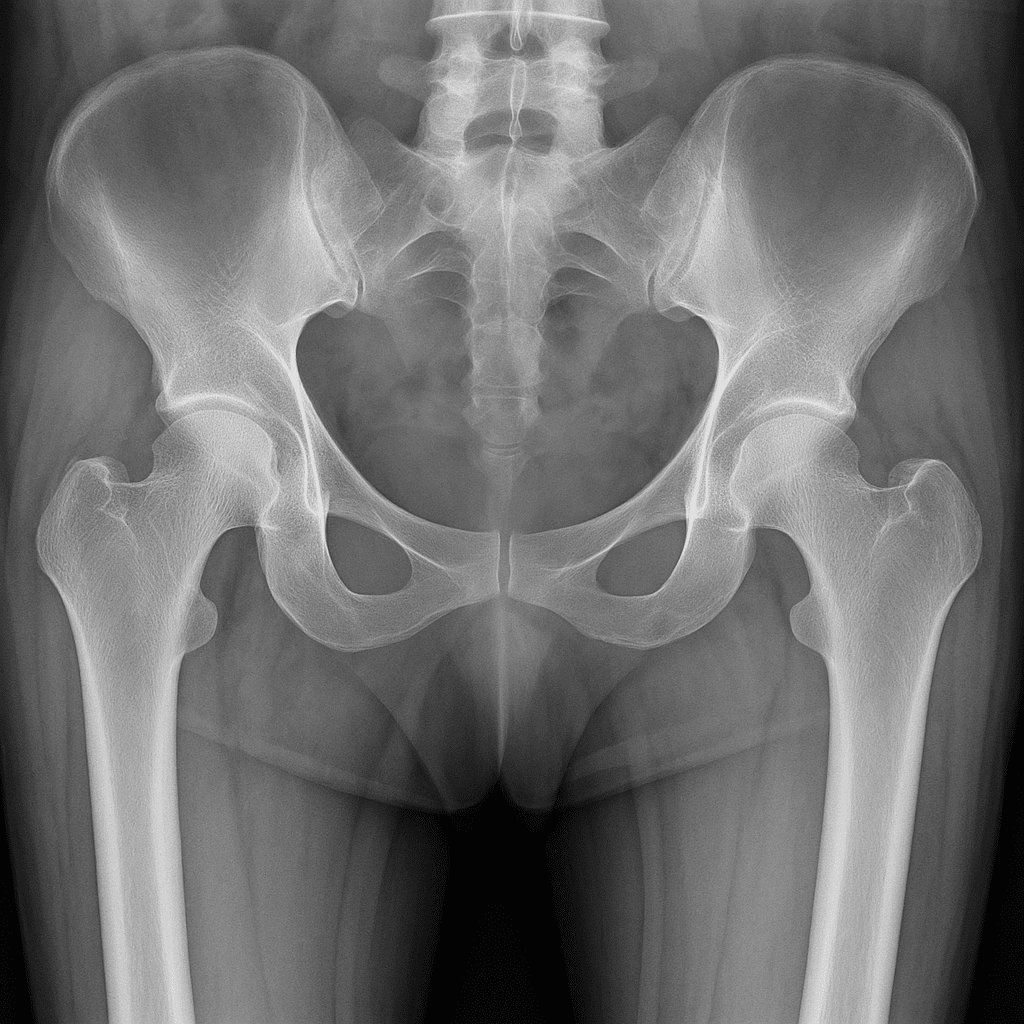
A ‘fragility’ fracture is a broken bone caused by a fall from a standing height or less. These fractures often affect older adults and are rising sharply, with over half a million cases annually across the UK. These injuries, often resulting from osteoporosis, lead to significant pain, disability, and loss of independence for patients. They also place immense pressure on the NHS, costing an estimated £2.2 billion each year. Therefore, it is important that we provide the best possible rehabilitation to enable people to return home, and to thrive at home after their fracture.
In response, Professor Katie Sheehan (Professor of Rehabilitation within the Centre for Bone and Joint Health at the Blizard Institute, Queen Mary University of London) is working with Barts Life Sciences to explore the impact of a pioneering data-driven approach to transform rehabilitation for older people recovering from these fractures. This work builds on Barts Life Sciences’ established expertise in translational research and reflects our commitment to moving innovation from bench to bedside, ensuring that patients benefit from the latest advances in care.
Over a 14-month period, the project – funded by UK Research and Innovation – explores the feasibility of using clinical natural language processing (NLP) to analyse rehabilitation from thousands of electronic health records (EHRs) from patients treated for hip, leg, and ankle fractures at Barts Health NHS Trust. The NLP will be used to ideally identify which approaches led to the best outcomes for patients.
Therapists typically record rehabilitation assessment and treatment using free-text notes. However, these notes do not follow a specific structure which limits the potential for researchers to analyse the data and extract the information required to improve rehabilitative care after a fragility fracture. The use of NLP provides the opportunity to unlock the ‘black box’ of this data. That means, the text will be analysed for common rehabilitation activities undertaken by patients, such as walking practice, exercise, and support with daily tasks. These will then be compared between patients and over time, allow scientists and clinicians to see what works best to support the rehabilitation of patients. This insight will help shape NHS guidance and drive best practice to improve the treatment of these patients.
Importantly, supported by the public and patient involvement group ‘TROOP’ (Trauma Rehabilitation [Orthopaedic] for Older People), the initiative ensures that patients and carers are involved at every stage, from shaping research questions to sharing findings widely.
This project positions the Centre for Bone and Joint Health, Barts Life Sciences, and North East London as a leader in bone & joint rehabilitation research and innovation, exemplifying how collaboration and the use of data can drive prevention and better outcomes for patients.
If you are an industry or academic partner interested in shaping the future of AI-driven healthcare, connect with us to tell us more about your idea.

 Accessibility options
Accessibility options Translate the page
Translate the page