Saving limbs with AI: How smart systems spot diabetic foot risks before it’s too late
Every year in England, more than 9,000 leg amputations are carried out due to complications from diabetes. Patients who undergo amputation face significant physical challenges, such as substantially reduced mobility and the need for prosthetic adaptation. Emotionally, many experience grief, anxiety, or depression as they adjust to life after limb loss and navigate changes in independence and identity.
Amputations also place significant financial pressure on the individual. The NHS covers basic prosthetics and rehabilitation, but individuals often need to fund advanced prosthetics, home adaptations, and ongoing therapy themselves. In addition, many experience a loss of income due to reduced work capacity or career disruption, further compounding the financial burden which might also affect their families. Amputation also places significant pressure on the NHS through costly surgical procedures, prolonged hospital stays, and extensive rehabilitation services.
Diabetes is one of the fastest-growing health issues in the UK and people with diabetes are 15 times more likely to undergo an amputation than those without the condition. Over 5.8 million people in the UK live with diabetes – including 4.6 million diagnosed cases (90% type 2 diabetes), an estimated 1.3 million undiagnosed, and more than 6.3 million at risk – bringing the total affected or at risk to over 12 million adults.
The Challenge
In North East London more than 150,000 people live with type 2 diabetes and in some of the boroughs in which our patients reside, the percentage of people living with type 2 diabetes is above the national average, making this challenge even more urgent.
This calls for bold, coordinated action and presents a unique opportunity for Barts Health NHS Trust to lead the way in prevention, innovation, and system-wide learning that can benefit the patients we serve.
In our local communities, many patients face barriers to regular care, due to a young transient population, diverse ethnicity and unequal access to healthcare as a result of cultural and systemic barriers. This makes it harder to manage blood sugar and detect complications early.
One of the most serious complications of diabetes is diabetic foot disease, which can lead to infections and, in severe cases, amputations. National guidelines recommend that every adult with diabetes admitted to hospital should have their feet checked and, if needed, be referred to a specialist multidisciplinary diabetic foot team within 24 hours of a foot problem being identified. However, due to attention being focussed on the serious medical problem for which the patient was admitted the foot problem might not be identified immediately, leading to a delay of the referral.
The Solution
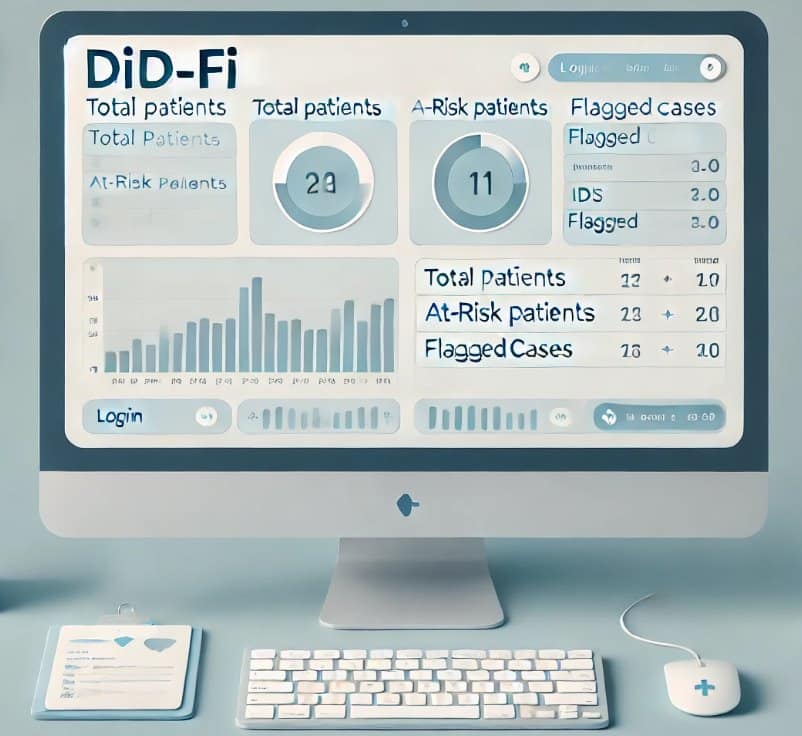
Barts Life Sciences, a partnership between Barts Health NHS Trust and Queen Mary University of London, developed an AI-powered digital dashboard to identify patients at risk of diabetic foot problems. The system uses natural language processing (NLP) to scan clinicians’ notes in electronic health records, searching for signs of diabetes and foot-related issues using SNOMED CT, a global standard for medical terminology.
The dashboard then flags patients it identifies as potentially having diabetic foot based on available clinical indicators. A podiatrist then reviews the alerts and arranges an assessment within 24 hours if needed. This means clinicians no longer have to manually search through thousands of records. Instead, the system does the heavy lifting, ensuring the right patients get the right care at the right time.
The Impact
In a two-month pilot at Barts Health, the system delivered impressive results:
- 87 patients were flagged for review, of which only 8 were previously known to the specialist team.
- Nearly 20% of the patients were flagged by the model as being at risk of having severe issues requiring urgent attention. These were all flagged correctly and the patients required urgent attention.
- 80% of patients were flagged as being at risk of mild diabetic foot. In 65% of these cases, the risk was confirmed. In 35% of the cases, patients were identified as not being at risk of having diabetic foot.
This approach not only reduced the risk of patients with diabetic foot from being missed but also gave clinicians confidence by showing exactly why a patient was flagged. What would have taken clinicians over 100 years to review manually was achieved in minutes.
This project demonstrates how AI can help us to use our time more effectively and place more emphasis on prediction and prevention, reducing the number of amputations and saving the NHS vital resources.
What’s Next
Going forward, we will apply our learnings from this study and aim to scale the trial to better train the AI model to identify patients who might have diabetic foot. We also hope to explore applications to identify patients at risk of peripheral arterial disease, diabetic neuropathy or other diabetic related complications moving towards a stronger focus on preventive, personalised, and evidence-based care.
If you are an industry or academic partner interested in shaping the future of AI-driven healthcare, connect with us to tell us more about your idea.

 Accessibility options
Accessibility options Translate the page
Translate the page